Vault prolapse surgery: When is it the right time?
Vault prolapse surgery is an important procedure for women who are suffering from pelvic organ prolapse. It can help reduce the pressure on pelvic organs, restore the normal anatomy of the vagina, and improve quality of life. However, this surgery can be complex and it is important to understand when it is the right time to have vault prolapse surgery. In this blog post, we will discuss the factors that should be considered when deciding if vault prolapse surgery is right for you.
What is Vault Prolapse?
What are the symptoms of Vault Prolapse?
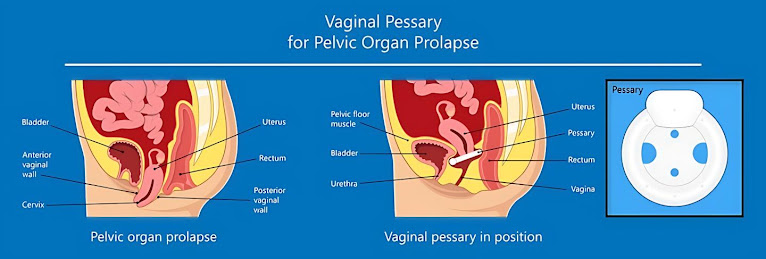
Vault prolapse is a condition in which the top of the vagina drops down and protrudes from the opening of the vagina. It is a type of pelvic organ prolapse, where one or more organs descend from their normal position in the pelvic cavity.
The most common symptom of vault prolapse is a bulge or protrusion at the vaginal opening. Other symptoms may include discomfort during sexual intercourse, feeling of fullness in the vagina, urinary leakage, constipation, and difficulty with urination. In some cases, there may also be an increase in vaginal discharge or an unpleasant odour.
Vault prolapse can also cause discomfort when standing, sitting or walking. Women may experience pain in their pelvis, back or lower abdomen that may be worse during or after intercourse. If you experience any of these symptoms, it’s important to speak to your doctor as soon as possible for diagnosis and treatment.
When is Vault Prolapse surgery done?
Vault prolapse surgery is typically done when the patient has not responded to non-surgical treatment methods and continues to experience significant discomfort or pain. Surgery may also be recommended for patients with recurrent urinary tract infections, difficulty emptying the bladder completely, or persistent bleeding. It is important for patients to weigh the risks and benefits of vault prolapse surgery before making a decision.
The decision to proceed with vault prolapse surgery is typically based on the severity of symptoms and the patient’s overall medical condition. Generally, surgery is recommended when the prolapse is causing severe pelvic discomfort or when there are signs of organ damage or obstruction. In most cases, the patient’s doctor will order a series of diagnostic tests including a physical examination, cystourethroscopy, and ultrasound to determine the extent of the prolapse.
In some cases, vault prolapse surgery may be delayed or avoided if other treatments such as lifestyle changes, medications, or physical therapy are found to be effective in treating the symptoms. Surgery should only be considered after all other options have been exhausted and the patient has experienced significant improvement in symptoms.
Ultimately, the decision to proceed with vault prolapse surgery should be made in collaboration with the patient’s doctor, taking into account the individual’s health history, age, and activity level. The risks and benefits should be carefully considered before making a final decision.
The surgical procedure
Vault prolapse surgery is done in a hospital or an outpatient center under general anesthesia. The exact method of surgery will depend on the severity of your prolapse, your general health, and other factors. Commonly used techniques include sacrospinous ligament fixation and uterosacral ligament suspension.
In a sacrospinous ligament fixation procedure, the surgeon will first use sutures to attach the top of the vagina to the sacrospinous ligament, which is a strong ligament located near the tailbone. This helps to stabilize the top of the vagina, allowing it to remain in its normal position.
Uterosacral ligament suspension is another common technique used for treating vault prolapse.
During this procedure, the surgeon will attach sutures to the top of the vagina and then secure them to the uterosacral ligaments, which are strong ligaments located in the lower abdomen and near the spine. This technique helps to provide additional support for the vaginal walls.
In some cases, the surgeon may recommend using a vaginal pessary to help manage symptoms. A pessary is a device that is placed inside the vagina and helps to provide additional support and keep the vaginal walls in their normal position.
After the surgery, you may need to use a vaginal dilator to help stretch the vagina, which will help with healing. You will also need to avoid sexual intercourse for at least six weeks after surgery, and you may need to use a lubricant during intercourse when it is eventually resumed.



Comments
Post a Comment